Reviewed Book
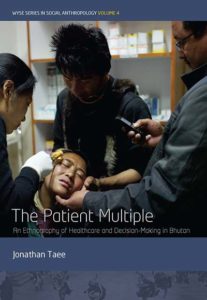
The Patient Multiple: An Ethnography of Healthcare and Decision-making in Bhutan. Jonathan Taee, New York: Berghahn Press, 2017, 220 pp.
In The Patient Multiple, Jonathan Taee offers the first ethnographic exploration into patient health care–seeking behavior and healing narratives in Bhutan. While his focus is on patient subjectivities, Taee aims to provide an understanding of how patients and their health care–seeking narratives are affected by the contexts that frame their diagnosis, treatment, and illness understandings. To that end, he provides readers with both a novel, well-defined understanding of the notion of patienthood and an overview of the multiplicity of practices available for patients in contemporary Bhutan. Taee’s 12 months of participant observation, formal and informal interviews, and focus groups took place in and around hospitals in Thimphu, the capital, and the eastern town of Mongar.
The book starts with a useful introduction, providing background to the country and situating recent health care changes within its broader sociopolitical context. Taee also introduces the three health care assemblages he identified in Bhutan by following individuals through their healing journeys and their particular histories within the country. He strategically uses the term “assemblages” instead of systems to steer away from rigid and finite categorizations. Two of these assemblages are state run and therefore institutionalized. These are the biomedical route and the traditional medicine services route. In reaching a hospital, a patient is asked to decide between one and the other. Along with these forms of care, the third assemblage people draw on is what Taee labels “alternative practices,” which may include shamanistic rituals, bone-setting, religious ceremonies, oracle use, spirit possession, dietary behaviors, and familial care (p. 5).
Through the personal healing journey and narrative of a female patient, Pema, Taee’s first chapter presents the theoretical crux of the book. Here, Taee leans on Mol’s concept of “body multiple” (2002) to assert that patienthood is enacted and emerges in the engagement with the multiple practices and cures available, resulting in a “patient multiple,” composed of and engaging with many healths and bodies. Taee then structures each of his subsequent chapters in a way that adds a new focus and understanding of the emergence of patients multiple and their health care decision-making behavior.
The focus of the second chapter is traditional medicine services. Taee observes the ways in which these services are being institutionalized, nationalized, and professionalized in order to be incorporated into the relatively recent national health care service project. He further argues that as a result of a relatively recent two option health care state service, a new way of being Bhutanese is being created, in the form of “bio-traditional citizenship.”
The third chapter cuts across assemblages and sheds light onto the processes of decision-making in the context of healing practice plurality. It is a powerful chapter that grounds patients’ lived struggles in two ethnographic cases: that of a newborn that was not feeding and that of a young girl with chronic arm pain. Taee exposes the messiness of the decision-making process and notices emerging ethical discourses such as patient responsibility around what an appropriate health care–seeking behavior entails (e.g., when, where, how, and why to seek which treatment).
Chapter 4 revolves around the non-institutionalized, alternative assemblage of healing practices and how these affect experiences of illness. In Bhutan, alternative healers are not isolated. Indeed, patients often seek and engage their healing practices. Taee provides an in-depth ethnographic exploration into a specific disease category, ja né, that surfaced regularly and emerged across distinct healing assemblages. Although he explains the biomedical and traditional categories of interpretation of ja né, his aim in Chapter 4 is to provide a detailed description of an alternative healing method that was said to have healed someone from ja né in Mongar. The practice involves the healer sucking the disease from the genitalia of both male and female patients. Despite the many controversies surrounding this practice, there is a strong demand for them. For Taee, this demand exemplifies the competency of patients to actively and agentively manage multiplicity among controversial opinions.
Finally, Taee explores how the materials of healing influence healthcare decision-making. While pharmaceuticals have been increasingly available over the past decade in Bhutan, Taee was present during a bottleneck of drug supply due to changes in a drug regulation policy. He uses the story of a tragedy that occurred during this drug shortage to argue that patients’ expectations of care from the biomedical assemblage, as well as ideas of what is clinically possible, have shifted. The chapter concludes with some practical suggestions for the Ministry of Health and other health care services. Surprisingly, in making these suggestions, Taee suddenly shifts his tone. Throughout the book, he is careful to steer away from rigid categorizations that would fail to account for the distinct ways in which patients enact and experience health care. Further, he seeks to keep boundaries fluid (e.g., between practices, and in talking of assemblages instead of systems) and to remain neutral in his judgment of those practices. In providing suggestions, however, Taee speaks of educating the Bhutanese population with appropriate knowledge to “display a more effective and timely response to illness” (p. 183), and he includes his own ethical judgment on right or wrong health-seeking behavior.
This shift in tone raises another question.
Obtaining access and research permissions in Bhutan is no easy endeavor. In fact, Taee is explicit about the difficulties and the excruciating, lengthy process he underwent to be able to carry out his research. He refers to the Ministry of Health and the National Traditional Medicine Hospital as research collaborators, and he acknowledges his collaborators’ influence on the ultimate focus of his research. The ethnography is beautifully grounded in several individual lives, and Taee was ultimately afforded ample access to health professionals, institutions, families, and events. Nevertheless, one cannot help but wonder about the influence Taee’s research collaborators had on the final product.
The book ends with a sober concluding chapter highlighting the fact that patients’ experiences of healing are created not only by the practices with which they engage, the distinct health concepts they use to make sense of their illness, or the bodies that emerge, but also by the ways “they manage, layer, sort, order and relate their patient multiplicity” (p. 192). Making health care decisions in a practice-plural context is not easy; however, Taee argues, drawing again from Mol (2008), that patients in Bhutan make decisions based on a “logic of care” instead of a “logic of choice.” In other words, the difficulty for patients resides in the assemblage, navigation, and management of patient multiplicity rather than in the stark choice between practices.
The Patient Multiple is a refreshing account of healing narratives in a medical plural context. It is a wonderful and insightful read, written in a way that is accessible to a wide audience, blending rich description and grounded analysis. Furthermore, beautiful photographs taken by the author accompany and complement the text. In sum, the book is very well suited for students at both undergraduate and post-graduate levels and is an important contribution for those interested in medical pluralism and the shifting healing landscape in the Himalayan region.
References Cited
Mol, A. 2002. The Body Multiple: Ontology in Medical Practice. Durham: Duke University Press.
Mol, A. 2008. The Logic of Care. Health and the Problem of Patient Choice. New York: Routledge.