Dmitrii was exhausted and in pain. Russia had launched its full-scale invasion of Ukraine just weeks ago, on February 24, 2022, and the 55-year-old spinally injured wheelchair user knew he had to leave Kyiv. Bombs were falling on the city. He hadn’t slept in weeks, and his sore foot was starting to swell. But there were no wheelchair accessible shelters. In early April, a well-connected friend got Dmitrii in a medical convoy evacuating Ukrainians with disabilities to the European Union.
Others in the convoy were taken to Germany, but Dmitrii (not his real name) had longed to live near the sea, so he chose northern France. They gave him a small, sunny room at an assisted living facility. Friends thought him lucky: a peaceful setting, three meals a day, sophisticated (and free!) health care. Dmitrii, a bachelor who had fled alone, had won the refugee lottery.
A little over two years later, having endured seven major surgeries including one to remove his bladder and another to amputate his leg, Dmitrii told me, “It’s hard to come to France and see only hospitals and lose half my body.” Four weeks later, Dmitrii died in a French hospital.
Dmitrii was not counted as a casualty of Putin’s war on Ukraine. But he was, indeed, a victim of two kinds of violence: the violence of war (the fast violence of warfare, and the slow violence of displacement), and curative violence (too much medicine). How did immigration and temporary asylum become a death sentence for this disabled war refugee? What went wrong?
*************************************
I met Dmitrii in Kyiv in the early 2000s. We got together and communicated regularly, and he was a prominent figure in my 2010 book Disability and Mobile Citizenship in Postsocialist Ukraine. Over time, he became like a brother to me, and in fact could have been since we were born only five years apart. From the time of Russia’s full-scale invasion until his death, Dmitrii and I exchanged thousands of social media messages and talked for around 25 hours on video chat. Shortly before he died, I visited him in northern France for several weeks of exploratory participant observation and informal interviews to conceptualize a new research project exploring the experiences of disabled Ukrainians who, like Dmitrii, had fled to other EU countries.
Any story of Dmitrii’s life and death will be hopelessly incomplete. After a tree fell on his spine while working in forestry (he was 22 years old), Dmitrii used a wheelchair for 35 years. In Ukraine he competed in wheelchair racing and basketball, led an advocacy organization for youth with disabilities, and mentored others with spinal injuries. He earned a university degree in rehabilitation. His default mode was humor: jokes helped him deflect serious talk and cope with pain. Dmitrii was addicted to cigarettes and was known to drink heavily at times. Reckless with friendships, he trusted some people too much and others too little. He loved the country of his birth—Ukraine—but identified ethnically and culturally as Russian, an unpopular political stance for the times.
For 28 months in France, Dmitrii communicated in Russian using a free oral interpretation app on his phone that “translated” his speech into French. His communication often got garbled as the system was imperfect at best. Staff at his residence identified communication—in both practical and cultural senses—as Dmitrii’s greatest challenge as a refugee. He still lived mentally and socially in Ukraine, filling his small room with gifts from home, mostly familiar foodstuffs like tins of fish, bricks of halva, and his favorite loose-leaf teas. His free time revolved around communicating with friends from Ukraine, many of them also refugees of the war.

As soon as he arrived in France, appointments with urologists, oncologists, cardiovascular specialists, vascular surgeons, and dentists hijacked Dmitrii’s days. Health problems erupted one on top of another. Dmitrii estimated that at least half of his 846 days in France were spent in a hospital, many in a blur of pain. More than once, medical students were convened at his bedside: “Doctors visit my room as if on excursion…they observe me, ask questions, poke me, and write something down.” Dmitrii joked that he was “a living miracle, a medical wonder.” His friends back home wondered if he wasn’t a guinea pig.
Soon after he settled in France, Dmitrii’s sore foot turned gangrenous. Years prior he’d had similar problems with his other leg, ultimately leading to a below-the-knee amputation. Having lived with a disability for 35 years, Dmitrii knew his own body and health history. He begged the surgeon to proactively amputate his second, worsening leg, also up to the knee. This would nip the problem in the bud and give him the option of being fitted with two identical prostheses, ideal for preserving his center of gravity in a wheelchair. But Dmitrii’s knowledge was not in a form that the French system of medicine valued.
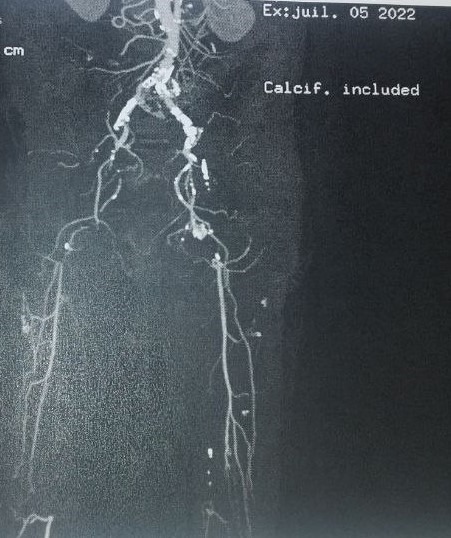
The surgeon wanted to “save the leg” through a two-part strategy: amputate just the one, worst gangrenous toe, and perform an atherectomy on Dmitrii’s aorta (the body’s largest artery) to improve circulation to his leg and foot. (Dmitrii called this “storming the blood clots.”) During the atherectomy Dmitrii’s arteries began to, in his words, “crumble like an anthill.” So the doctors replaced a large portion of his aorta in his chest and abdomen with synthetic tubes. Dmitrii joked that with one prosthetic leg and now a plastic aorta, he was becoming a cyborg.
Meanwhile, the extensive imaging performed on Dmitrii had revealed not just a series of blood clots, but a concerning shadow in his bladder—a tumor. The urologist operated immediately to remove the mass for biopsy. After weeks with no news, Dmitrii received a dreaded diagnosis: bladder cancer. The urologist recommended removal of the entire bladder; he wanted to perform a urostomy, which meant Dmitrii would pass urine through an opening (stoma) in his abdomen to an external pouch that he would need to empty every few hours. Dmitrii agreed, and the urostomy took place three weeks later.
Dmitrii was unprepared for the scrupulous attention a urostomy required. The urine tubes had a mind of their own and the “waterproof” pouch was anything but. His leaky body was depressing. He felt his physical independence slipping away. And the urine bag dealt a blow to his manhood: he couldn’t imagine ever going to bed with anyone again. The residence staff called a psychologist. When Dmitrii refused to talk about anything other than his lost sexuality, the psychologist didn’t come back. Adding insult to injury, a nurse’s post-surgery error caused one of his testicles to turn black and swell horribly. It nearly burst, and he was rushed back to the hospital for emergency surgery.
Dmitrii was sent to rehabilitation after he regained some strength. He hadn’t walked in 35 years. On rare occasions he had pulled himself to standing. After his L2 compression fracture 35 years prior, he had been warned by other spinally injured people about “ambitious” doctors, would-be “heroes of medicine” who’d try to “get him back on his feet.” Nevertheless, he was surprised by their ableist methods: “They are teaching me to walk!” he texted me one day. But the “light course” of “walking” rehabilitation was disastrous. Again, his blood vessels crumbled. His foot, the one the surgeon had heroically “saved,” turned blue. It started to rot. The blueness crept up Dmitrii’s leg.
The surgeon wanted to amputate the whole leg, all the way up to the hip. Dmitrii was in shock, especially since he had asked for a below-the-knee amputation pro-actively when he had first arrived. An emergency amputation ensued. Due to infections and circulation problems, one major surgery turned to three in quick succession.
For years, Dmitrii’s Ukrainian doctors had forbidden any procedures with general anesthesia—he was a stroke survivor with blood clots. But during his 28 months in France, Dmitrii had six surgeries under general anesthesia, and a seventh under local. His medical care—free for a refugee with temporary protection—cost the French state hundreds of thousands of Euros. Occasionally Dmitrii pondered returning to Ukraine to his familiar doctors, but his thoughts were tangled. “French medicine saved me,” he thought, and, “medicine in Ukraine is only focused on the war wounded, they’ve no time for ‘regular’ disabled people like me.”
In his last days of life, Dmitrii was dealing with a major infection at the stump of his amputated leg, an expansive, infected pressure wound on his buttocks, and the threat of kidney failure from major complications with his urostomy. Exhausted and “tired of hospitals and doctors,” Dmitrii asked for pain management only. Then, in an all-too-familiar hospital room, in a morphine-induced coma, he slowly slipped away.
Thinking of Dmitrii’s experience as “dislocated biology”—what happens when a unique organism relocates to a novel setting—helps me explain if not fully comprehend his untimely death. Anthropologist Margaret Lock wrote about “local biologies,” the “manner in which biological and social processes are permanently entangled throughout life, ensuring a degree of biological difference among humans everywhere that…at times bears profoundly on well-being.” Dmitrii’s unique disabled body was managed in a thoroughly Ukrainian medical and social context for 35 years. In Northern France, the language, the food and drink, the cool, damp climate, and the ideas about disability and in/dependence were unfamiliar to Dmitrii. When his singular biology crossed borders and was subsumed to a new (French) local context, the consequences were necessarily unpredictable and unfortunately for Dmitrii, disastrous. Stress also played a role. As we sat together on his patio in late June 2024, I asked Dmitrii what he thought had caused his rapid deterioration after immigration. He answered:
“I was stressed by the behavior of people who feared bombs dropping on them at any moment and who were on the edge of hysterics. It was up to me to constantly be a psychologist and keep everything under control, to prevent nervous breakdowns. Then the trip to the middle of nowhere and uncertainty about my status…When things calmed down, all my ‘frozen’ (Rus. zakonservirovannye) illnesses began to squirm out of me.”
Most of Dmitrii’s complaints were not novel to his French context: after all, he’d had blood clots, urinary tract problems, and infections in Ukraine, too. Health problems plagued him regardless—a stroke, liver cancer—and he always refused to die. But the French health care system proposed more invasive interventions. On the one hand, Dmitrii told me he was impressed by the extensive medical tests he received, especially ultrasounds, radionuclide imaging, and MRIs. On the other hand, these tests made his anomalies visible and “known,” which inevitably triggered invasive procedures that Dmitrii poorly understood. These led to cascading side effects and follow-on interventions that he could not anticipate. He was ambivalent: “I trust the doctors here,” Dmitrii said, but he felt poorly informed about treatment plans and follow-up.
Even as he endured these unfamiliar medical regimes, Dmitrii pursued more familiar treatments from home. Friends shipped him medicine from Ukraine that he incorporated into his treatment, probably unbeknownst to the French doctors. Many Ukrainians living in Europe prefer Ukrainian health care and visit their home country for “medical tourism.” This option was not available to Dmitrii as a person with serious disabilities and no means to pay for travel.
I do not know if medical professionals in France were particularly motivated to “care harder” for Dmitrii out of sympathy for his plight and Ukraine’s. But I do know that the profound disability expertise Dmitrii had accumulated as a spinally injured wheelchair user was not valued. Few were aware of his university degree in rehabilitation. Providers evinced little interest in his personal history, how he had lived and survived in Ukraine, and what interventions had heretofore kept him alive. Biomedicine by its nature involves unequal power relationships between doctor and patient, but Dmitrii experienced an extreme: his status as a migrant allowed for the erasure of his personal histories. This deepened his already profound biological and cultural dislocation.
In medical settings, even at a time of immense global sympathy for displaced Ukrainians, a civilizational discourse positioned France as a civilized, European nation, and Ukraine as an uncivilized, “nowhere” nation. This discourse drove a process of cultural-medical imperialism whereby treatment was bestowed on Dmitrii, a supposedly less capable cultural-medical subject with no expertise and little agency. He questioned the civilizational-imperialist stance that enabled French doctors to practice “heroic medicine” on him. The misguided attempt to “save the leg,” and a rehab regime to get a spinally injured person “walking:” these were pathways for doctors to enhance their reputations, not to provide treatments that were in Dmitrii’s best interest.
These dynamics subjected Dmitrii to curative violence, “violence that is made invisible in the name of cure.” Curative violence often has an imperialist nature, when a state wields “its power to cure disabled others and to offer international assistance to ‘those in need.’” Even as Ukraine’s European credentials were touted in the context of Russia’s war, it was regarded as an uncivilized, peripheral country, and Dmitrii was positioned as the beneficiary of “advanced” French medicine.
It was precisely in ignoring Dmitrii’s underlying disability that French doctors wielded fatal curative violence. Dmitrii remarked that doctors treated him as a “regular, healthy person” with specific medical problems (blood clots, poor circulation, urinary tract irregularities). Instead, they should have considered his baseline condition—a longtime wheelchair user with an L2 compression fracture: “I’m the first spinally injured person they’ve treated here. These doctors know nothing about spinal cord injury.” Here was another layer of invisible violence wrought by displacement and immigration policies: Dmitrii admired the bucolic French countryside where he lived, but his choices for healthcare there were limited.
Few realized the extent of Dmitrii’s solitude: he was completely alone in France, with no supportive close ones, save a few staff members at his residence who spent countless hours assisting with forms, transport, communication, and other tasks of daily living. Dmitrii was not in a zone of social abandonment: over time he received helpful social and nursing services. But as a lone refugee without fluency in the French language, bureaucracy, or medical system, Dmitrii desperately needed forms of forceful, permanent advocacy that he did not receive.
Dmitrii’s doctors and therapists overlooked (or dismissed) his one absolute priority: to remain physically independent for as long as possible. He often expressed this to those close to him, including me. In Ukraine Dmitrii had remodeled his own house in a way that kept him physically independent; the full-scale invasion that damaged it and compelled him to flee had ruined his independence and hard work. The violence of disconnection between Dmitrii’s body and the habituated, bodily-adjusted environment of his house compounded his dislocated biology.
When the space of opportunities shrinks, people with disabilities often improvise with their bodies. The new realities Dmitrii faced in migration restricted his space for improvisation and constrained his agency to make choices about his bodily experiences. Dmitrii arrived in France a single, middle-aged disabled war refugee with only a wheelchair and a backpack. He could not predict his future and from his perspective, could not afford to become dependent on physical assistance and technical supports. His encounter with French medicine and rehab was a constant negotiation about independence.
What might a treatment regime that prioritized Dmitrii’s fierce wish for independence have looked like? Could a designated health care advocate have made a difference? Would a capable French-Russian interpreter have enabled more culturally appropriate, patient-centered care? What if his doctors had valued Dmitrii’s disability expertise that had made survival possible in Ukraine? Could a treatment plan have been negotiated that accounted for Dmitrii’s dislocated biology, his lived experience, and his lifestyle priorities?
Dmitrii was cared for in France. Particularly moved by his status as a single war refugee, staff at his residence moved hell and high water to connect him to services. He praised “good nurses” and doctors’ noble intentions. Dmitrii’s friends abroad were rocks of encouragement. But these forms of care, however generous, were no match for the curative violence heaped upon him. Dmitrii fled the violence of war only to encounter medical violence packaged as Care.
This story of the dark underbelly of care does not do justice to Dmitrii, his resilient spirit, or his capacity to love and care. There are many more stories to be told of Dmitrii. But this is the one that needs telling right now.
*************************************
Postscript: On August 13, 2024, Dmitrii’s French friends—staff from the facility where he had lived—scattered his ashes in the North Sea. This was according to his wishes.

Acknowledgements: I am grateful to Frances Bernstein, Maria Bucur, Evguenia Davidova, Maria Cristina Galmarini, Julie Hemment, William R. Morris, Jr., Volha Verbilovich, Hanna Zaremba-Kosovych, Natalia Pamula, Kate Wiegele, Magdalena Zdrodowska, and MAQ editors Alex Nading and Jessica Robbins-Panko for their contributions to this article and its arguments.
Sarah D. Phillips is Professor of Anthropology at Indiana University-Bloomington, where she also teaches for the Human Biology Program.