Reviewed Book
Reimagining Social Medicine from the South. Abigail H. Neely, Durham: Duke University Press, 2021, 169 pp.
Reimagining Social Medicine from the South. Abigail H. Neely, Durham: Duke University Press, 2021, 169 pp.
Casey Golomski
University of New Hampshire
Social medicine is a branch of medicine concerned both with the biology of disease and social determinants of health. Its focus has been on the intersecting roles that material and socioeconomic inequalities and state policies play in the maldistribution of disease. Much of its most effective and internationally celebrated and replicated treatment and prevention outcomes are based in community-based research and primary health care. The movement for social medicine gained traction in the early 20th century, when critically minded doctors, policymakers, and revolutionaries sought to alleviate public health crises of the poor associated with industrialization, capitalism, and other modern ills. In states around the world, it began to take root.
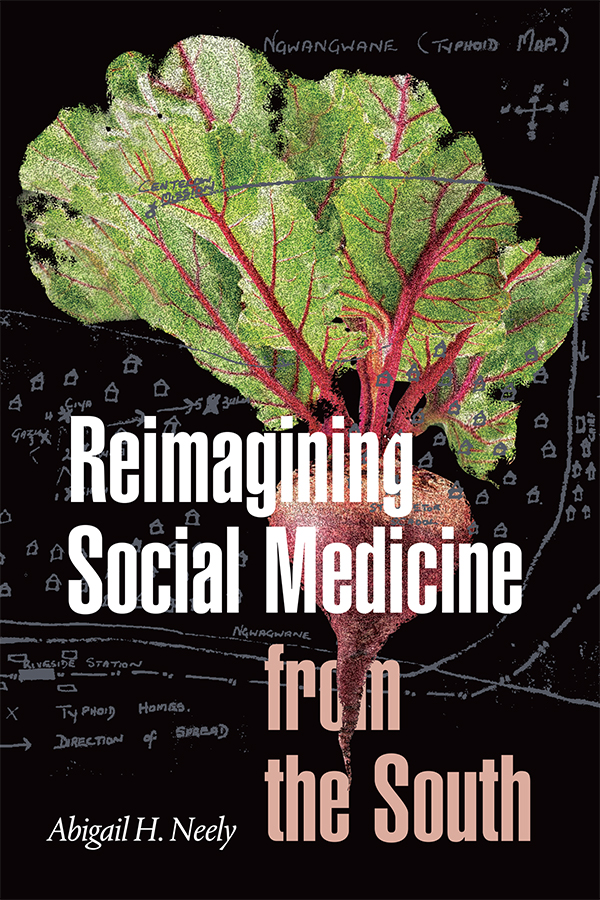
Another root—a beet—and its leaves hover transparently above a map depicting a typhoid outbreak in a rural South African community on the cover of Abigail H. Neely’s Reimagining Social Medicine from the South. Beetroot is a key symbol of South Africa’s commensal cultures and its history of health care. It stands for everyday gendered sociality as a main ingredient bought or farmed by women to make for funeral feasts. It stands for state-driven HIV/AIDS mortality as a moniker for the former Minister of Health Mantombazana Tshabalala-Msimang, who promoted it as a form of good nutrition instead of providing antiretrovirals nationally in the 2000s. In Neely’s book, it also stands for one of the many micronutrient-rich species first introduced by social medicine’s practitioners in the 1940s in the Zulu-speaking area of Pholela when they saw that its residents suffered from malnutrition induced by migrant labor and land dispossession—themselves outcomes of racial capitalism.
In theory, the beet also stands for much more. Reimagining Social Medicine from the South takes a political ecological approach to understand the successes and challenges of implementing social medicine—in this case, in the historic project of the Pholela Community Health Center (PCHC). PCHC, founded by anthropologically trained, Marxist-influenced Drs. Sidney and Emily Kark and colleagues in 1940, was meant to improve health in a proto-apartheid Native Reserve area. For Neely, a political ecological approach means seeing “health and healing as ontological and constitutive of worlds” (p. 10) where illness and wellness are physical manifestations of entanglements among relationally produced human and nonhuman beings.
These beings include doctors and (as) researchers, patients and (as) research subjects (the focus of Chapters 1 and 2), nonbiomedical illnesses sent by abathakathi (witches) and izangoma’s(healers) ritual and herbal remedies treat them (the focus of Chapter 4), and all varieties of animals and plants in the environment, including longer term agricultural staples and newer, nutritionally vital food species (the focus of Chapter 3)—such as beets. She builds this approach by synthesizing theories of racial capitalism, structural violence, actor networks, assemblages, and medical pluralism from the critical and methodological perspectives of feminist geography and science studies. Beets and other beings call “attention to the more-than-human, place-specific relationships that make people sick and that can make them better” (p. 104).
The bookis based on qualitative and document research in South Africa and the United States. Neely’s field research took place in and near the PCHC catchment area and much was done with Thokozile Nguse, with whom she has also published about the ethics of research relationships (one of many social relationships, including more than human ones that make up a world, the subject of Chapter 2). Together, they interviewed older adults in two communities within the original catchment area and one outside. Altogether, they gathered oral histories from eight households about health and livelihoods between 1955 (the justification for this start year is unclear) and 2009 (the year after Neely’s first field trip). Six photographs of the participants and landscape help illustrate the contemporary communities inheriting the legacy of social medicine.
The document research is impressive and constitutes most of the information presented in the book. Neely reviewed PCHC archival documents at Wits University and South Africa’s National Archives, as well as the corpus of literature produced by the Karks and subsequent generations of PCHC researchers. Neely offers detailed descriptions of how the PCHC team conceptualized and operationalized their social scientific research and medical practice to understand health across individual, household, community, and national levels—effectively a multi-scalar approach. She includes several impactful historic cases that confounded doctors—residents’ refusals to treat tuberculosis, for example, when doctors disregarded lived experiences of abathakathiin the case of Khanyisile (pp. 85–88)—to show the limits of social (bio)medicine. Four images of PCHC archival documents also help illustrate these interventions in the landscape.
Much has been written about the history, challenges, and successes of the social medicine model as it was developed in South Africa (in the case of PCHC) and applied worldwide (including in Israel, the United States, and the 1978 Alma-Ata Conference). Neely’s book will be especially useful for graduate students and professionals working with the large body of existing literature on health interventions like this and need a strong model for how to rework this literature in exciting critical and theoretical frames. I can also imagine successfully using Chapter 3 (Nutrition, Science, Racial Capitalism) in undergraduate medical anthropology or global public health courses to show how structural racism perpetuates food insecurity to then impact health.
With illustrative figures, detailed descriptions of clinical and field research reports, and rich ethnographic and historic context, Neely effectively writes “from Pholela” as an historic and place-based articulation of social medicine as she aims to do in the introduction. In what perhaps befits this kind of political ecological or geographic approach, there are far fewer quotes from contemporary Pholela residents describing the world in their own words—her interactions with gogos (grandmothers) Sithole (pp. 42–45) and Ngcobo (pp. 1–2) stand out in this respect. The book makes sure that readers learn that social medicine is an ontological formation that involves more-than-human social relationships. This means emphasizing and clearly tracing more-than-human relationships themselves among multiple beings, forces, and historic moments where they manifest in clinical and political ecological view—rather than describing peoples’ own reflective engagements on these relationships in which they come to see themselves as human and in pursuit of wellness among these beings (Huhn 2020). Black Southern Africans like Khanyisile and gogos Sithole and Ngcobo have long had their humanity denied before, during, and now after apartheid, something Neely also clearly shows. In reading this book alongside Black geographies—such as McKittrick and colleagues’ (2015) reviews of Sylvia Wynter’s work on humanness as an outcome of racialization, space, and time—the next iteration of this political ecological approach might be to ask: What are humans and nonhumans in social medicine, when do they become such, and for whom?
References Cited
Huhn, A. 2020. Nourishing Life: Foodways and Humanity in an African Town. New York: Berghahn.
McKittrick, K., ed. 2015. Sylvia Wynter: On Being Human as Praxis. Durham: Duke University Press.